What if the key to understanding complex diseases lies within our cells and how closely we can mimic them in the lab? This question has driven researchers to improve cell models, particularly in the context of the intestine and diseases like inflammatory bowel disease (IBD). The journey toward better models is a fascinating blend of innovative science and collaborative efforts.
The Limitations of Traditional Cell Models
Drug development heavily relies on simplified cell culture models. These models allow for scaled testing of new drugs; however, they often fall short in accurately portraying the complexities of cells as they exist in the body. When minimized to a lab dish, vital aspects of cellular function can be lost. This gap in fidelity leads to significant consequences: promising candidates fail in clinical trials, and critical cellular targets are overlooked.
Does this mean that researchers are at a dead end? Not at all! The technological advancements in cell modelling are opening up new avenues of understanding.
The Role of Advanced Techniques in Cell Modelling
One of the groundbreaking technologies leading the charge is high-throughput single-cell RNA-sequencing. This method allows scientists to examine gene expression at the level of individual cells, effectively creating a comprehensive map of cellular function. When the researchers at MIT and Harvard applied this method to the intestinal cells, they made substantial discoveries regarding how well existing cell culture models mimic actual cells in the body.
Understanding the Unique Characteristics of Intestinal Cells
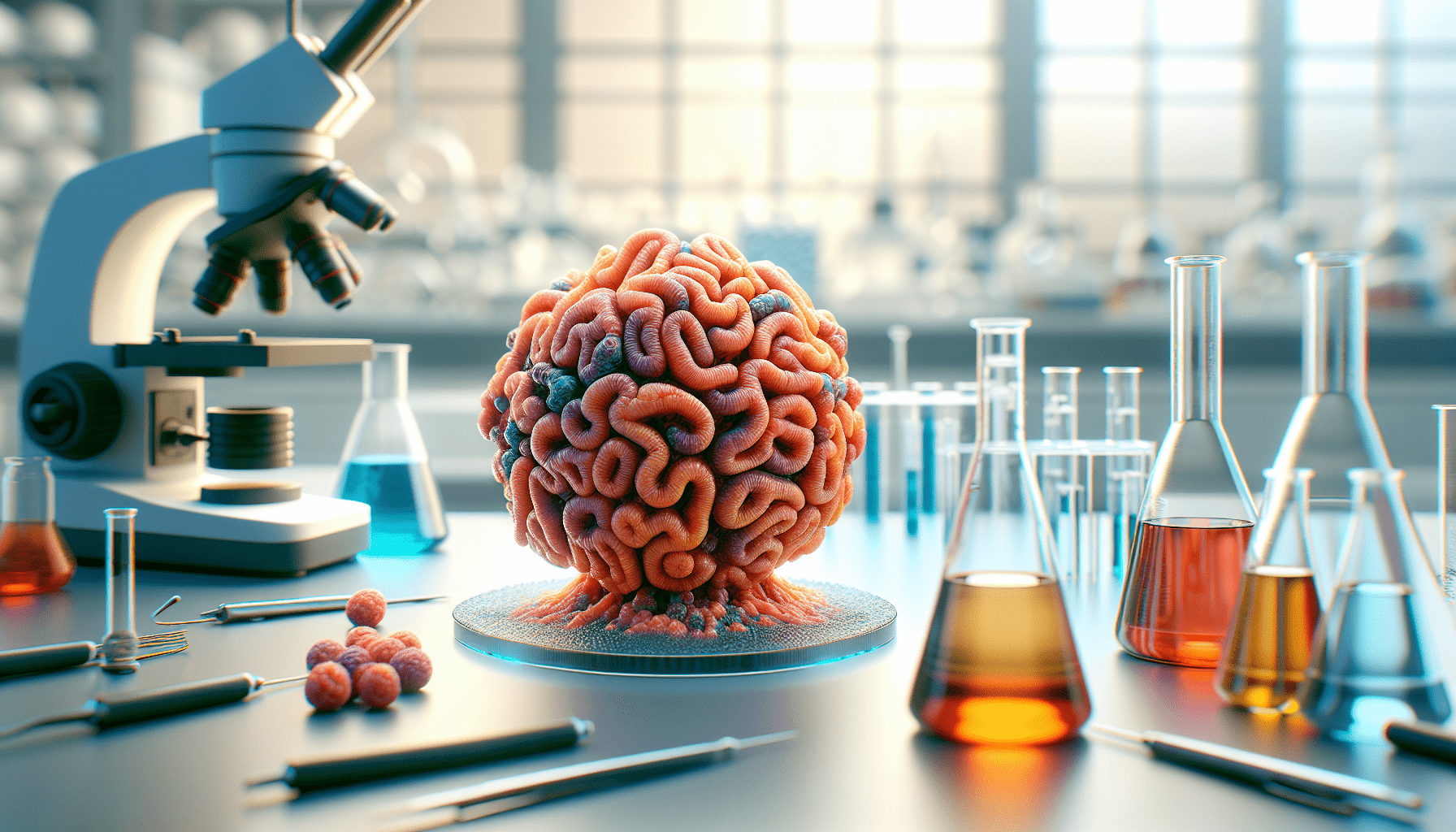
In the study, the researchers compared single-cell RNA-sequencing data from a mouse’s small intestine to data derived from organoid models of the same tissue. Organoids are remarkable 3-D structures formed from adult intestinal stem cells, but they may not fully capture the diversity of cell types found in a natural setting.
Through this comparative analysis, they were able to isolate specific cell types and evaluate how well these organoid-derived cells matched their in vivo counterparts. This examination highlighted the gaps in traditional models and ignited a push for improvements rooted in actual biological data.
Collaborations That Drive Innovation
Leading this collaboration were talented researchers from various institutions, including Ben Mead, a doctoral student, and Jeffrey Karp, a professor at Brigham and Women’s Hospital. It’s important to highlight that the progress in creating improved models comes from teamwork across disciplines—biological engineering, medical sciences, and data analysis come together in this effort. Their work not only benefits the study of IBD but also has implications for understanding other diseases related to cellular dysfunction.
Unpacking Genetic Risk at the Cellular Level
With the rise of single-cell RNA-sequencing, mapping the activities of “risk genes” has become feasible. These genes may contribute to diseases like Crohn’s disease, a form of IBD. Understanding where these genes orchestrate action within tissues—and ultimately at the single-cell level—is crucial to developing novel therapeutic interventions.
This mapping effort can be likened to a treasure hunt; the ultimate goal is to locate the “X” that indicates where corrective therapy may be applied.
Advances in Single-Cell RNA-Sequencing Technology
At MIT, advancements in single-cell RNA-sequencing established a new benchmark for studying tissues with low input clinical samples. It allows researchers to dissect complex tissues and identify critical patterns of gene expression. This economical approach enables the profiling of tens of thousands of cells, shedding light on the genetic makeup necessary for discerning cell types in various conditions.
Importance of Mapping Specific Gene Expression
Mapping tissues is paramount in pinpointing where risk-related genes operate. The process of translating this understanding into practical applications hinges on developing representative models of the identified cell types. Notably, the Paneth cell—a cell type essential for gut health—is a key player in studies focused on genetic risk and IBD.
By having a detailed map of the true characteristics of the small intestinal cells found in nature, researchers can develop models that authentically represent these cells.
The Paneth Cell: A Central Player in IBD Research
Genetic studies have previously highlighted the role of Paneth cells in defending against pathogens and maintaining stem cell niches within the intestine. In traditional cultures, replicating these cells has posed significant challenges, largely because the organoid models did not quite align with real intestinal cells. This misalignment can lead researchers on incorrect paths in their search for effective drug targets.
Re-Engineering Cell Development Pathways
Scientists aspire to create models that reflect the realities of biology, and with the new insights gained from single-cell data, the researchers have begun correcting gaps in the developmental pathways of Paneth cells. The synthesis of cellular models that closely resemble actual cells promises to create more reliable platforms for testing therapeutics.
Through this innovation, they successfully generated Paneth cells that not only closely mimic their natural counterparts but also function effectively in their roles—killing bacteria and supporting stem cells.
Transitioning to Clinical Applications
With advancements in generating more authentic cell types, the researchers are now focusing on creating practical applications. Mead, who aims to continue this innovative work, is developing a screening platform to investigate Paneth cell biology in greater detail.
The Broad Implications of Improved Cell Models
As the integrity of models improves, the implications extend beyond just understanding IBD. The methodologies created here can be utilized across a spectrum of organ-related research—liver, kidney, lung, and even brain. By providing a model that accurately resembles in vivo conditions, researchers can more effectively examine disease mechanisms and identify potential therapies.
Understanding Disease Biology and Accelerating Therapeutics
A core objective of this research is to enhance our grasp of fundamental disease biology. This effort inevitably leads to faster development of therapeutic options. Key insights derived from accurately designed cell models are vital for ushering in the next generation of medical solutions.
The Future of Cell Model Development
As this initiative progresses, it reveals that the fundamental understanding of how specific cell types express genes linked to disease is critical. It underscores the message that improved disease models must truly reflect the complexities of the cells they aim to represent.
This work may pave the way for breakthroughs not just in IBD but in various medical conditions where accurate cell representation plays a role in understanding and treatment.
Conclusion: The Path Forward
The intricate journey of creating better cell models of the intestine has just begun. As researchers combine cutting-edge technology with a collaborative spirit, the prospects for more effective therapies become increasingly promising. The hunger for a deeper understanding of our cellular health propels this journey forward, revealing new horizons in medical science.
In your quest to understand the landscape of cellular modeling, it’s important to recognize that each advancement brings us one step closer to overcoming the limitations of traditional approaches. As the understanding of how diseases manifest at the cellular level deepens, so too does the potential for holistic treatments that can transform patient care.