Ever wondered about blood vessels in the brain that don’t connect right? These issues aren’t usually passed down through genes. Yet, they pose a big health risk for many people of all ages. Arteriovenous malformations (AVMs) are complex conditions where blood vessels get tangled. This creates bad connections between arteries and veins.
This messes up blood flow, leading to tissues not getting enough oxygen. It can also cause serious problems like bleeding, stroke, or brain damage.
Women might notice AVM symptoms during pregnancy. Risk factors include high blood pressure and other vascular issues1. Most people with brain AVMs are between 20 and 50 years old. Many don’t show any symptoms1.
When symptoms do appear, quick treatment is key to avoid serious problems.
Key Takeaways
- AVMs are complex neurovascular conditions characterized by improper blood vessel connections.
- They commonly affect individuals aged 20 to 50, often without noticeable symptoms1.
- Symptoms could emerge during pregnancy due to increased blood pressure1.
- Treatment is crucial to prevent severe complications like hemorrhage and stroke.
- The importance of specialized medical teams, like those at Seattle Children’s Vascular Anomalies Program, cannot be overstated due to their expertise2.
To learn how stem cell therapy technology is a good solution For any Health Challenge – contact us at stemboostx @ gmail.com with subject ” Techtest “.
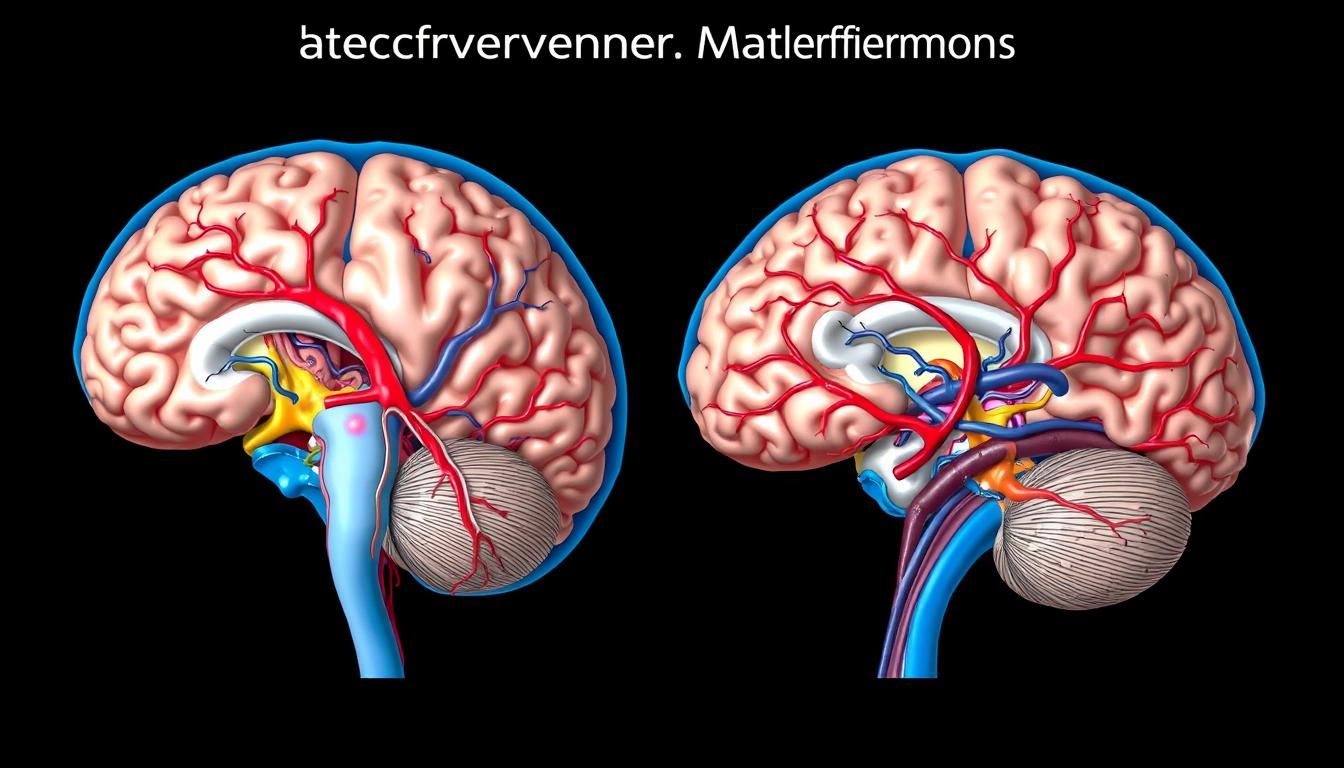
What are Arteriovenous Malformations?
Arteriovenous malformations (AVMs) are a congenital vascular defect. They involve abnormal connections between arteries and veins, skipping the capillary system. This leads to brain problems and malformations.
AVMs are usually found in people in their mid-30s. But, they can appear as early as birth3. The chance of an AVM rupturing in the brain is about 2-4% each year. But, different AVMs can have different rupture rates4.
Definition and Basic Understanding
AVMs are a congenital defect with direct artery-vein connections. These vessels are not good for exchanging nutrients and oxygen. About 50% of people with AVMs first show symptoms with a bleed.
Other symptoms include seizures, muscle weakness, headaches, and memory problems4. AVMs are rare, happening in about 1.12 to 1.34 per 100,000 people5. Most AVMs don’t show symptoms at first, but about 45% of those that do start with a bleed5.
How AVMs Disrupt Blood Flow
AVMs disrupt blood flow by letting arterial blood flow directly into veins. This skips the capillary network, leaving tissues without enough oxygen. Over time, this can weaken blood vessels, increasing the risk of rupture.
Ruptures can lead to severe health issues like hemorrhagic strokes. AVMs with deep venous drainage and aneurysms are at higher risk of bleeding4. Even though AVMs are rare, their impact on the brain is significant. Early detection and treatment are crucial to prevent serious complications4.
Symptoms of Arteriovenous Malformations
It’s important to know the symptoms of arteriovenous malformations (AVMs) for early treatment. Most AVMs don’t show symptoms, but when they do, they can be very dangerous.
Neurological Symptoms
AVMs can cause serious neurological problems. Symptoms include losing brain function, seizures, headaches, and confusion. About 12 percent of people with AVMs show symptoms, and less than 4 percent have a serious bleed6.
Other symptoms include vision problems, strange feelings, and brain fog7. Pregnant women might see symptoms get worse because of blood changes7. Also, about half of brain AVM cases start with a bleed8.
Physical Symptoms
Physical symptoms of AVMs can be serious. They include muscle weakness, paralysis, vision issues, dizziness, and developmental problems in kids7. Severe cases can lead to brain damage and oxygen loss8.
People might also have trouble speaking, moving, and even lose consciousness7. But, less than 1 percent of AVM cases are fatal7.
AVMs are complex and can affect both brain function and physical health. Learn more about AVMs and new treatments being tested.
Causes of Arteriovenous Malformations
The exact causes of arteriovenous malformations (AVMs) are still a mystery. Yet, we’ve found some factors that might play a role. By looking into genetic changes and environmental triggers, we’re getting closer to understanding AVMs.
Genetic Factors
Most AVMs aren’t passed down through families9. They often appear at birth10. While genetic changes, like hereditary hemorrhagic telangiectasia, can increase the risk, they’re not common. Issues during blood vessel formation can also lead to AVMs.
Environmental Triggers
Environmental factors can also cause AVMs, sometimes right after birth or later10. Events like puberty, pregnancy, or trauma might trigger them. This shows how genetics and environment can work together. AVMs can also appear suddenly, without a family history9.
To learn how stem cell therapy technology is a good solution For any Health Challenge – contact us at stemboostx @ gmail.com with subject ” Techtest “.
Risk Factors Associated with Arteriovenous Malformations
Arteriovenous malformations (AVMs) are complex blood vessel problems. They can cause serious health issues. Knowing the risks helps catch problems early, preventing big problems like bleeding or brain damage.
Family History
Most AVMs happen by chance, but family history matters. If your family has AVMs, you might be at higher risk. Studies show a 3% chance of bleeding in the brain each year5.
Getting checked early if you have family history can help a lot.
Hereditary Conditions
Some hereditary conditions like hereditary hemorrhagic telangiectasia (HHT) or Osler-Weber-Rendu syndrome increase AVM risk. About 5% of AVM cases are linked to these conditions11. Knowing your genetic risk is key, as these conditions can lead to many complications.
AVMs have a 2% chance of bleeding each year if they haven’t bled before. If they have bled, the risk jumps to 4.5%5. Doctors need to watch patients with these conditions closely.
Research shows AVMs affect 1.12 to 1.34 people per 100,000, with 88% being hidden5. But, when they show symptoms, 45% bleed, highlighting the need for careful monitoring5. For those with HHT or Osler-Weber-Rendu syndrome, regular check-ups and specific plans are crucial to reduce risks.
Complications Arising from AVMs
Arteriovenous malformations (AVMs) pose serious risks if not treated. These risks include bleeding and damage to the brain. Knowing these risks helps in early detection and treatment.
Bleeding and Hemorrhage
Bleeding in the brain is a major complication of AVMs, often leading to stroke12. When an AVM ruptures, it can cause severe brain damage or even death12. In children, AVMs are a leading cause of hemorrhagic stroke12.
AVMs can also surprise patients with their severity, especially when found during other treatments12.
Women face higher risks during pregnancy due to increased blood volume and pressure12. Postoperative bleeding is a concern, but it’s rare after 24 hours13. New surgical techniques, like Thulium laser, offer hope in reducing these risks13.
Neurological Damage
AVMs can cause a range of neurological problems, from abnormal sensations to memory loss12. Surgery can also lead to neurological deficits if the brain’s important areas are damaged13. Inaccurate bleeding control after surgery can cause complications13.
Small bleeds can accumulate over time, leading to dementia and cognitive decline12.
Imaging tests like MRI are key in planning and checking surgery to avoid neurological damage14. Tools like intraoperative fluorangiography and ultrasound doppler help remove malformations completely13.
- Symptoms: abnormal sensations, dizziness, headache, seizures, memory loss, muscle weakness, visual disturbances12.
- Complications: direct lesion of eloquent areas, postoperative bleeding, postoperative hyperemia13.
- Diagnostic methods: angiography, CT scans, MRA, MRI, functional resonance121314.
Diagnosis of Arteriovenous Malformations
Diagnosing arteriovenous malformations (AVMs) involves several steps. Advanced imaging tests and detailed clinical exams are key. Each step is crucial for accurate diagnosis and treatment planning.
Imaging Tests
Imaging tests are vital in diagnosing AVMs. MRI, CT scans, and angiography are used to see the malformations’ size, location, and details. MRI scans give a clear view of the brain and spinal cord, helping spot AVMs precisely.
In the last 30 years, imaging has improved a lot. This has almost doubled the number of people found with unruptured AVMs4. Early detection and better management are now possible. Many AVMs are found by chance during scans for other health issues154.

Angiography, which uses dye to see blood vessels, is also important15. It shows how blood flows through the AVM. This helps find weak spots or missing capillaries.
Clinical Examinations
Clinical exams are just as important as imaging tests. They check cognitive, motor, and sensory functions. These exams help see how the AVM affects a person’s health.
About 12 percent of people with AVMs have symptoms like seizures, headaches, and muscle weakness4. Doctors use these exams to plan the best treatment. This way, every part of the patient’s condition is checked, leading to better care.
Treatment Options for Arteriovenous Malformations
Treating Arteriovenous Malformations (AVMs) involves managing symptoms and preventing complications. Methods range from simple watchful waiting to advanced interventional radiology techniques like embolization and sclerotherapy. Surgery is often the main treatment, especially when there’s a high risk of bleeding16.
Embolization is a common treatment that involves injecting a substance to block parts of the AVM. This reduces blood flow17. Stereotactic radiosurgery is another option that uses precise radiation beams to stop abnormal blood flow18. These treatments are often used alongside medical management to manage symptoms, as there’s no cure for AVMs yet.
Patients have regular check-ups to see how well the treatment is working and to catch any complications16. In some cases, AVMs might not be treated right away. Instead, patients are closely watched with yearly imaging and clinical follow-ups to ensure they’re safe18.
For those looking for more treatment options, there are clinical trials for new surgical and non-surgical methods. Microscopic surgery can cure AVMs that are accessible, helping patients recover faster17. After surgery, recovery takes two to six months, with activity restrictions for four to six weeks. The surgery can have side effects like stroke, seizure, and problems with speech or memory18.
If you’re interested in new treatments for AVMs and other health issues, contact our team. Reach out at stemboostx@gmail.com with the subject “Techtest” to learn about the latest interventional radiology techniques and medical management strategies for relief and recovery.
Surgical Interventions for AVMs
Surgical options are often needed for AVMs that cause symptoms or are at high risk. The chance of bleeding from an AVM can be as high as 8% each year. This shows why quick action is crucial19. The size and location of the AVM help decide the best surgery plan.
Embolization Procedures
Embolization is a treatment where materials block the abnormal blood flow in an AVM. This makes the AVM smaller and less likely to bleed. It’s especially helpful before surgery, making the operation easier19.
Using embolization with other treatments can help shrink the AVM by 11-40%20. It’s also part of a plan for treating bigger AVMs, often before surgery or radiation.
Stereotactic Radiosurgery
Stereotactic radiosurgery uses targeted radiation to slowly shrink an AVM. It’s best for AVMs that are about 3 cm or smaller20. It’s a good choice for AVMs rated Spetzler-Martin grade I or II if surgery is too risky20.
Combining radiosurgery with embolization can lead to better results, even though the AVM might not disappear completely20. For more on AVM treatment, check out the Mayo Clinic’s website19.
FAQ
What are arteriovenous malformations (AVMs)?
Arteriovenous malformations (AVMs) are complex conditions in the brain. They are made of tangled blood vessels that skip the capillary system. This can cause problems like not enough oxygen to tissues and bleeding.
How do AVMs disrupt blood flow?
Blood in AVMs goes straight from arteries to veins, skipping capillaries. This means tissues don’t get enough oxygen and nutrients. It can weaken blood vessels and lead to strokes.
What are some symptoms of arteriovenous malformations?
Symptoms of AVMs vary and can be serious. They include seizures, headaches, and confusion. Muscle weakness, vision problems, and headaches are also common. In severe cases, it can cause bleeding and be life-threatening.
What causes the development of arteriovenous malformations?
The exact cause of AVMs is not known. They are usually present at birth and develop during blood vessel formation. Genetic mutations or environmental factors might play a role.
Are there risk factors associated with arteriovenous malformations?
Yes, having a family history of AVMs or certain hereditary conditions increases risk. Knowing these risk factors helps in early diagnosis and treatment.
What complications can arise from AVMs?
Complications include bleeding, seizures, and severe neurological damage. A ruptured AVM can be fatal. Chronic bleeding can also lead to dementia and cognitive problems.
How are arteriovenous malformations diagnosed?
Imaging tests like MRI, CT scans, and angiograms are used to diagnose AVMs. These tests show the malformation’s size and location. Clinical exams also assess overall health.
What treatment options are available for AVMs?
Treatment options include watching the condition (conservative management) and interventional radiology. Techniques like embolization and sclerotherapy are used. Medical management is also used to manage symptoms, but there’s no cure.
What does surgical intervention for AVMs involve?
Surgical treatments include embolization and stereotactic radiosurgery. Embolization blocks abnormal blood flow, and radiosurgery shrinks the AVM over time. Treatments are tailored to each case based on the AVM’s characteristics.
Source Links
- https://www.brighamandwomens.org/neurosurgery/arteriovenous-malformations – Arteriovenous Malformations Diagnosis and Symptoms
- https://www.seattlechildrens.org/conditions/avm/ – Arteriovenous Malformations – Seattle Children’s
- https://rarediseases.org/rare-diseases/arteriovenous-malformation/ – Arteriovenous Malformation – Symptoms, Causes, Treatment | NORD
- https://www.aans.org/patients/conditions-treatments/arteriovenous-malformations/ – Arteriovenous Malformations
- https://www.ncbi.nlm.nih.gov/books/NBK531479/ – Arteriovenous Malformations of the Central Nervous System – StatPearls
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/arteriovenous-malformations – Arteriovenous Malformations
- https://www.ninds.nih.gov/health-information/disorders/arteriovenous-malformations-avms – Arteriovenous Malformations (AVMs)
- https://www.mayoclinic.org/diseases-conditions/brain-avm/symptoms-causes/syc-20350260 – Brain AVM (arteriovenous malformation) – Symptoms and causes
- https://www.mayoclinic.org/diseases-conditions/arteriovenous-malformation/symptoms-causes/syc-20350544 – Arteriovenous malformation – Symptoms and causes
- https://medlineplus.gov/arteriovenousmalformations.html – Arteriovenous Malformations | AVM | MedlinePlus
- https://www.aaroncohen-gadol.com/en/patients/arteriovenous-malformation/types/risk-factors – Arteriovenous Malformations Risk Factors
- https://www.ucsfhealth.org/conditions/arteriovenous-malformation – Arteriovenous Malformation
- https://www.ncbi.nlm.nih.gov/books/NBK573750/ – Complications in AVM Surgery – Trends in Cerebrovascular Surgery and Interventions
- https://emedicine.medscape.com/article/248456-overview – Practice Essentials, Background, History of the Procedure
- https://www.barrowneuro.org/condition/arteriovenous-malformation-avm/ – Brain Arteriovenous Malformation (AVM)
- https://www.mayoclinic.org/diseases-conditions/arteriovenous-malformation/diagnosis-treatment/drc-20454895 – Arteriovenous malformation – Diagnosis and treatment
- https://www.mountsinai.org/locations/cerebrovascular-center/conditions/vascular-malformations/brain – Arteriovenous Malformations Treatments | Mount Sinai
- https://www.brighamandwomens.org/neurosurgery/arteriovenous-malformations-treatment – Arteriovenous Malformation (AVM) Treatment & Surgery
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5755136/ – Comprehensive Endovascular and Open Surgical Management of Cerebral Arteriovenous Malformations
- https://emedicine.medscape.com/article/1160167-treatment – Medical Care, Surgical Care, Consultations